Introduction:
Ever wonder what happens to all of the data that is gathered during a clinical trial?
Who makes sure that each adverse event, lab result, and patient record is correct, safe, and compliant with regulations?
And how do the life-saving therapies we currently depend on get their start from this data?
Clinical Data Management (CDM) is an unsung hero that is responsible for every authorized medication, successful clinical study, and regulatory filing.
CDM makes ensuring that the millions of data points produced by clinical trials that take place across continents are clean, consistent, verified, and useful. It is the cornerstone of evidence-based medicine and is essential to the development of new drugs, patient safety, and successful regulatory outcomes.
What Is Clinical Data Management?
The gathering, integration, and confirmation of clinical trial data are all part of the specialist field of clinical data management, or CDM. In order to support regulatory clearances and strong scientific conclusions, CDM’s ultimate purpose is to guarantee that the data produced by clinical trials is accurate, comprehensive, dependable, and statistically sound.
To put it another way, CDM is the clinical research industry’s quality control engine, making sure that the appropriate data is collected, maintained safely, and used effectively and morally.
The Significance of Clinical Data Management in Clinical Trials
The purpose of clinical trials is to provide important answers on the effectiveness and safety of medical interventions. However, even if a treatment is revolutionary, the study as a whole may fail if the supporting data is faulty. This is where CDM comes into play. By upholding stringent regulatory criteria and preserving data integrity, CDM guarantees that:
There is no compromise on patient safety.
- Trial results are reliable.
- Submissions to regulations are accepted more quickly.
- Credibility of science is maintained
CDM is “the process of collecting, cleaning, and managing subject data in compliance with regulatory standards to support clinical trials and research,” according to the Society for Clinical Data Management (SCDM).
Source:
https://www.scdm.org/
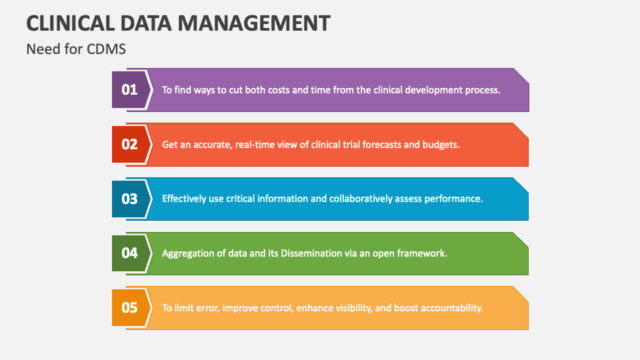
Clinical Data Management’s Primary Goals
- Ensuring Data Quality
- Reduce the number of data collection mistakes
- Verify and purify datasets.
- For transparency, provide audit trails.
- Preserve Patient Safety
- Early detection of irregularities or warning signs
- Make those adverse events are appropriately coded and tracked.
- Facilitate Adherence to Regulations
- Comply with international laws like ICH-GCP recommendations, FDA (21 CFR Part 11), and EMA
- Observe data protection regulations, such as the GDPR.
- Quicken the Development of Drugs
- Spend less time cleaning and balancing data.
- Make analysis and decision-making more rapid.
Important Elements of Clinical Data Management
| Component | Description |
| Case Report Form (CRF) | The main instrument for gathering trial data from every participant (either electronic or paper) |
| Electronic Data Capture (EDC) | A software framework that makes data management, validation, and collecting digital |
| Data Validation and Cleaning | The procedure for locating, fixing, and recording data mistakes or discrepancies |
| Medical Coding | Dictionaries such as MedDRA or WHO-DD to standardize terminology for illnesses, drugs, and events |
| Database Lock | The moment when information is deemed complete and prepared for statistical analysis |
| Audit Trail | A record of every update, user action, and data modification to guarantee integrity and traceability |
The Clinical Data Lifecycle
Throughout the course of a clinical study, CDM is an ongoing, systematic procedure rather than a one-time occurrence. This is a condensed illustration of how data moves through CDM:
- Examine Startup
- Describe the data collecting instruments (CRFs).
- Establish processes and standards for validation.
- Data collection
- Gather patient information from labs, EDC, and other sources.
- Data Cleaning
- Find mistakes, pose questions, and address discrepancies
- Data Coding
- Use standard dictionaries to code medical phrases.
- Reconciliation of Data
- Align data from various sources (such as lab results and EDCs).
- Archiving and Database Locking
- For the last analysis, freeze the dataset.
The Objective of Clinical Data Administration
Managing spreadsheets and software is only one aspect of CDM; another is making sure that the information obtained from clinical trial participants is:
- Accurate: Shows accurate, actual values.
- Complete: No information is omitted or missed.
- Reliable: Consistent throughout trial sites, time points, and systems.
- Compliant with regulations: Fulfils international requirements set by the ICH-GGP, EMA, FDA, and others.
Stakeholders, including sponsors, doctors, researchers, and regulatory agencies are able to make informed judgments on the safety and effectiveness of investigational goods because to this meticulous data processing.
Source: Quantzig
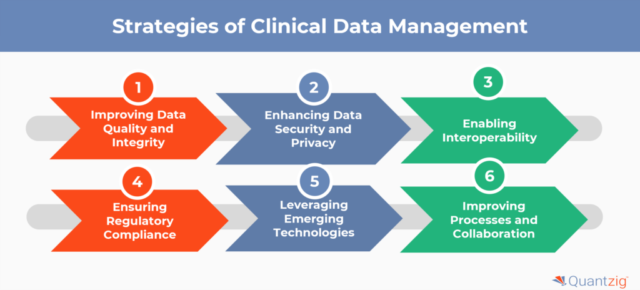
Key Clinical Data Management Activities
CDM comprises a number of vital tasks, including:
- CRF Design and Protocol Review
The CDM team works with clinical researchers to create Case Report Forms (CRFs) that comply with the study protocol before any data is even gathered. These forms specify the types, methods, and timing of data collection.
In the past, paper CRFs were the norm.
Nowadays, electronic CRFs, or eCRFs, are commonplace and are usually included in Electronic Data Capture (EDC) systems.
Source:
https://www.cdisc.org/standards/foundational/cdash
- Database Creation
Following the completion of CRFs, a clinical database is constructed to replicate the research design and gather data in real time during the experiment. Field definition, validation rules, edit checks, code dictionaries, and user access privileges are all part of this.
- Validation and Data Entry
Both automated edit checks and manual reviews assist guarantee quality when data is input, often using EDC:
- Range checks (for example, the ideal systolic blood pressure range is 90–200 mmHg)
- Checks for logic (for example, masculine respondents shouldn’t claim being pregnant)
- Absence of data checks (such as omitted required fields)
Data queries are used to identify and fix each discrepancy; site personnel handle these queries, and the CDM team keeps an eye on them.
- Medical Terminology Coding
Standard dictionaries like as the following are used to code data, including adverse events, drugs, and diagnoses:
- Regulatory Activities Medical Dictionary (MedDRA)
- WHO-DD, the WHO Drug Dictionary
Consistent analysis across trials and geographical locations is made possible by this standardization.
Source:
https://www.meddra.org/
- Reconciliation of Serious Adverse Events (SAE)
Clinical and safety databases must reconcile SAE data for safety reporting in order to prevent inconsistencies and guarantee prompt reporting to regulatory bodies.
- Data Cleaning and Review
Data managers collaborate with statisticians, medical reviewers, and monitors (CRAs) to clean the data by:
- Continuous evaluations of data
- Trend evaluations
- Risk-based evaluation of data quality
- Database Lock
A database lock is carried out once the data is judged to be complete, consistent, and clean. Changes cannot be done after this point. After that, the locked data is transferred for:
- Analysis of statistics
- Preparing a Clinical Study Report (CSR)
- Submission of regulations
Goals of Clinical Data Management
| Goal | Description |
| Data Quality | Ensure the highest standards of data completeness and privacy |
| Patient Safety | Enable real-time monitoring of efficacy and adverse events |
| Regulatory Readiness | Ensure that all data complies with FDA, ICH, GCP, and EMA guidelines |
| Operational Efficiency | Streamline data flow to reduce trial costs and delays |
| Auditability | Maintain full traceability with metadata and audit trails |
The Clinical Research Lifecycle and the Significance of Clinical Data Management
Clinical data management is intricately woven across a clinical trial’s whole lifespan and cannot be considered a stand-alone function:
- CDMs work together on system setup, CRFs, and protocol design at study startup.
- While conducting a study, CDMs keep an eye on incoming data, handle inconsistencies, and guarantee data quality.
- CDMs complete data, secure databases, and assist analytic teams throughout study close-out.
- Trials are vulnerable to delays, higher expenses, regulatory lapses, and even safety hazards in the absence of robust CDM procedures.
Fact:
One of the top five reasons for regulatory delays in medication approval procedures, according to research from the Tufts Centre for the Study of medication Development, is data-related problems.
Source:
https://csdd.tufts.edu/
Evolution of CDM: Then vs Now
| Then | Now |
| Paper-based data collection | Electronic Data Capture (EDC) |
| Manual query resolution | AI-powered query automation |
| Isolated systems | Integrated platforms (EDC + CTMS + ePRO) |
| Focused only on clinical trials | Includes virtual trials, wearables, and real-world data |
| Delayed data insights | Analytics and real-time dashboards |
Clinical Data Management: Who Does It?
Usually, a cross-functional team from pharmaceutical corporations does CDM.
- CROs, or contract research organizations
- Academic medical facilities
- Biotech companies
Important responsibilities consist of:
- Manager of Clinical Data
- Associate in Data Entry
- Programmer for databases
- Coder for Medicine
- Validator of Data
- Analyst of Data Quality
Regulatory Compliance and CDM
Clinical data management is governed by stringent international laws and moral principles, such as:
- ICH-GCP (Good Clinical Practice, International Council for Harmonization)
- U.S. FDA electronic records and e-signatures are governed under 21 CFR Part 11.
- GDPR (EU: Privacy of Patient Data)
- HIPAA (US): Protection of Patient Health Information
The traceability, auditability, and security of clinical data are emphasized in each law.
Source:
https://www.fda.gov/regulatory-information/search-fda-guidance-documents/part-11-electronic-records-electronic-signatures-scope-and-application
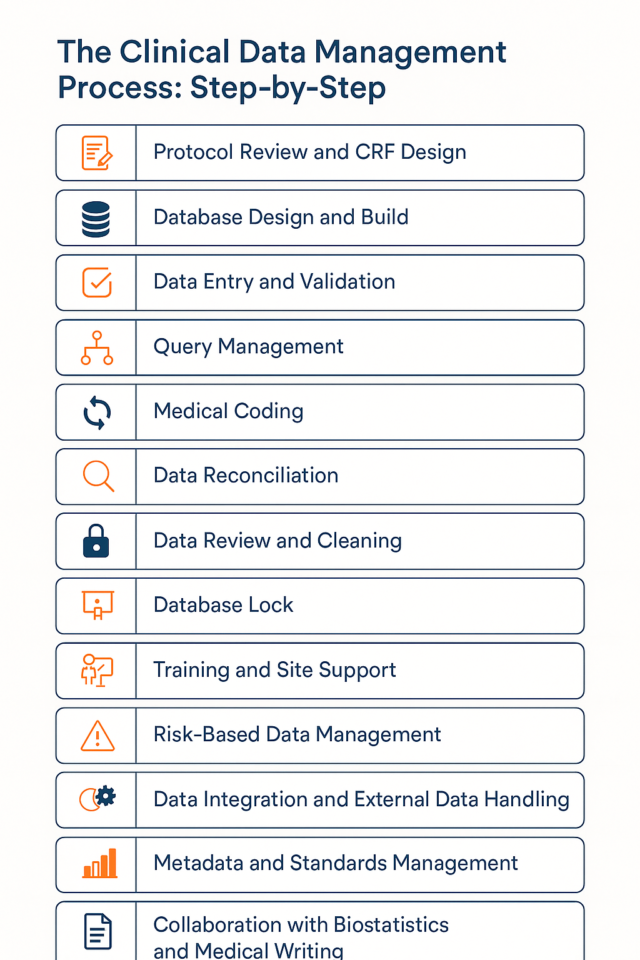
Clinical Data Management Process: Step-by-step
The multi-phase, painstaking process known as clinical data management (CDM) guarantees that the data produced during a clinical study is precise, consistent, timely, and verifiable. Every step of this process is interrelated and adds to the final dataset that regulatory bodies use to inform important healthcare choices.
Let us examine the people, instruments, procedures, and technology involved in each stage of the Clinical Data Management process in this extensive section of the blog.
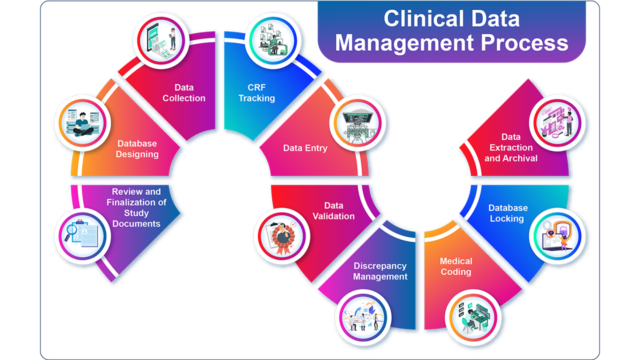
- Review of the Protocol and Study Setup
1.1 Development of Study Protocols
Any clinical trial’s basic document is the study protocol. It describes the goals, methods, statistical factors, and specifics of the operations. To make sure the data needs are precise, quantifiable, and in line with regulatory criteria, the clinical data management team examines the protocol.
- Important things to think about when reviewing a protocol:
- Primary and secondary endpoint identification
- Criteria for inclusion and removal
- Parameters for safety monitoring
- Timetables for visits and data gathering places
Clinical Data Managements guarantee that the information gathered will support both scientific publication and regulatory approval.
1.2 Design of the Case Report Form (CRF)
One tool for gathering data from clinical trials is the CRF. CDMs create comprehensive and easy-to-use CRFs in collaboration with CRAs and medical monitors.
CRF design steps:
- CRF annotations to connect each field to the data management strategy and protocol
- Standardization through the use of CDISC CDASH standards
- Free-text field minimization to cut down on discrepancies
- Explicit unit specifications and field definitions
Tools used:
Medidata Rave, Veeva Vault, Oracle InForm, and REDCap were the tools utilized.
Source:
https://www.cdisc.org/standards/foundational/cdash
- Design and Construction of Databases
Following the completion of the CRF design, an Electronic Data Capture (EDC) system is used to create a research database.
Database development steps:
- Configuring screens for data entry
- Defining automated data validations, or edit checks
- Derivations of programming data (e.g., BMI from weight and height)
- Including coding dictionaries (WHO-DD, MedDRA)
Database testing consists of:
- Individual module unit testing
- Testing integration for comprehensive data workflows
- Clinical and sponsor teams’ use of User Acceptance Testing (UAT)
The completed database has to be verified in accordance with GCP and 21 CFR Part 11.
Source:
https://www.fda.gov/regulatory-information/search-fda-guidance-documents/part-11-electronic-records-electronic-signatures-scope-and-application
- Information Gathering and Input
3.1 Course Enrollment
Data input utilizing the EDC system begins in real-time as locations start enrolling participants.
3.2 Verification of Source Data (SDV)
By comparing the data recorded in the CRF with the source documents (such as lab results and hospital records), monitors (CRAs) carry out SDV.
3.3 Best Practices for Data Entry
- After every visit, enter data as soon as possible.
- Prevent delays to speed up the answer to your questions.
- Observe the format and unit requirements (e.g., date formats).
Data from wearable devices is being used more and more, and remote data input is typical in decentralized studies.
- Data Validation and Cleaning
The foundation of CDM Clinical Data Management is data cleansing. By identifying outliers, missing numbers, and discrepancies, it guarantees data integrity.
4.1 Edit Checks That Are Automated
Inaccurate or missing data is flagged by preprogrammed rules:
- Range checks: Hemoglobin levels ought to be between 10 and 20 g/dL.
- Logic checks: A man shouldn’t disclose that he is pregnant.
- Checks for format: Dates must be entered in the format DD-MM-YYYY.
4.2 Manual Evaluation of Data
Clinical data reviewers manually evaluate data that has been highlighted and pose questions as necessary.
4.3 Management of Queries
Messages made to websites requesting explanation or correction are known as queries:
- Both automated and manual query creation are possible with systems such as Medidata Rave.
- Sites reply, and when a query is answered, data managers close it.
- Every modification has an audit trail according to GCP.
4.4 Reports on Data Discrepancies
Frequent reports aid in monitoring:
- Closed versus open inquiries
- Most common problems with data
- Performance of data input at the site level
- Coding for Medical Services
To maintain uniformity, medical words gathered during the study (such as adverse events and concurrent drugs) must be entered into accepted dictionaries.
5.1 Coding for MedDRA
Adverse event (AE) coding is done using MedDRA:
- Hierarchy that is standardized (SOC, HLGT, HLT, PT, LLT)
- Guarantees consistent reporting throughout research.
5.2 Coding for WHO-DD
Medications are coded using WHO-DD.
- Gives distinct identifiers to brand names and active compounds.
5.3 Coding: Automatic versus Manual
- An effort is made at auto-coding for precise text matching.
- For incomplete or unclear entries, a manual review is required.
Source:
https://www.meddra.org/
- Reconciliation of Serious Adverse Events (SAE)
The EDC and the pharmacovigilance (PV) system are often where SAE data is gathered. To guarantee the accuracy of safety reporting, disparities must be resolved.
The steps are:
- SAE line listings are generated from both systems.
- Finding discrepancies (e.g., severity, beginning date)
- Coordinating the resolution with safety teams
- Archival and Data Lock
7.1 Temporary Lock
Carried out to freeze subsets of data for analysis following significant milestones (such as the conclusion of therapy).
7.2 Locking the Database
Occurs following the resolution of all questions, the verification of all evidence, and the expectation that nothing will change.
Actions to take:
- Final analysis of data
- Lock and freeze data
- The lock should be noted in a trial master file.
7.3 Activities After Lock
- Create statistical datasets.
- Encourage the development of clinical study reports (CSRs)
- Archive information according to legal deadlines, which are usually 15–25 years.
- Compliance and Audit
Regular audits of Clinical Data Management operations are conducted to ensure compliance with:
- ICH-GCP
- Sponsor SOPs
- Regulations (such as FDA and EMA)
The audit checklist consists of:
- Logs of query resolution
- Logs of data validation
- Coding dictionaries
- Documentation for UAT
Correctional and Preventive Actions (CAPA) may be triggered by audit results.
- The Function of Automation and Technology
From paper forms to advanced digital systems, Clinical Data Management has changed throughout time.
9.1 Important Technologies
- EDC systems, such as Veeva Vault and Medidata Rave
- CTMS (such as Siebel CTMS from Oracle)
- Tools for Data Integration
- Dashboards for Risk-Based Monitoring
9.2 Machine learning and artificial intelligence
AI improves:
- Generate queries automatically
- AE detection via natural language processing
- Analytics that predict site performance

- Instruction and Site Assistance
Well-trained site personnel are the foundation of an effective Clinical Data Management. To guarantee that clinical site staff are aware of the protocol requirements, EDC systems, and data entry best practices, CDM teams offer organized training and ongoing assistance.
Important tasks include of:
- Making data entry guidelines and user guides
- Organizing site initiation visits (SIVs) and investigator meetings
- Providing both recorded and live training sessions
- Offering help desk assistance for urgent problems
Continuous interaction enhances the quality and speed of data entry while lowering data inconsistencies.
- Data Management Based on Risk
In order to organize and prioritize important data points, modern Clinical Data Management uses a risk-based strategy, which lessens the workload associated with thorough human inspection.
Some fundamental ideas are:
- Finding important information and procedures
- Creating KRIs (key risk indicators)
- Finding trends or outliers with statistical monitoring
- Concentrating SDV and DCF activities in high-risk regions
This method increases productivity without sacrificing data quality and complies with regulatory guidelines (such as ICH E6 R2).
- Integrating Data and Managing External Data
Data from many external sources, including central laboratories, imaging suppliers, ECG providers, and wearable technology, are frequently incorporated into trials.
The following are steps to manage external data:
- Creating Agreements for Data Transfer (DTAs)
- Creating common data formats, such as CDISC SEND, XML, and CSV
- Using secure FTP and APIs to automate imports
- Using EDC data for reconciliation
Planning for data translation, scheduling, and thorough testing are necessary for a successful integration.
- Management of Metadata and Standards
Interpretable and consistent datasets are made possible by metadata, or data about data.
CDM teams oversee standards like:
- Clinical data tabulation using CDISC SDTM
- CDISC ADaM for dataset analysis
- Terminologies under control, such as SNOMED and LOINC
- Common CRF libraries
Standards adoption guarantees quicker regulatory filings, enhances data exchange, and eliminates uncertainty.
- Cooperation with Medical Writing and Biostatistics
Clinical Data Management doesn’t function in a vacuum. To guarantee reliable, comprehensive, and analyzable data, it collaborates extensively with biostatistics and medical writing.
Points of collaboration include:
- Dataset preparation for both preliminary and final statistical analysis
- Assisting in the creation of summary tables and data listings
- Confirming that data and clinical accounts are consistent
- Supplying data documentation for regulatory filings and CSRs
This coordinated endeavor guarantees that data is not only hygienic but also appropriate for use in scientific and regulatory settings.
Clinical Data Management’s (CDM) Role Include:
In order to guarantee the availability, correctness, and integrity of clinical trial data, clinical data management, or CDM, is essential. The CDM function collaborates closely with stakeholders in the clinical, statistical, regulatory, and technological domains to support every stage of a clinical trial, from study design to data submission. An extensive examination of the main functions of CDM is provided here, along with real-world examples and references.
| Role | Description | Real-World Example | Key Tools/Standards |
| Protocol Interpretation and CRF Design | Convert clinical procedures into organized instruments for gathering data. | CRFs for oncology trials that are in line with CTCAE for AE monitoring | CDISC CDASH, Medidata Rave |
| Database Design and Build | Provide verified platforms for data entry that include derivations and edit checks. | Pfizer’s quick development of a COVID-19 database | Veeva Vault, Oracle InForm |
| Data Entry Oversight | Check the correctness and timeliness of site data entry. | Studying dermatology remotely while validating images | OpenClinica, SAS, JMP |
| Query Management | Create, monitor, and address data inconsistencies with websites | 98% query closure is achieved in a rare illness experiment. | Medidata Rave, Query dashboards |
| Medical Coding | Use WHO-DD and MedDRA to standardize terminology for worldwide reporting. | Diabetes trial coding variants of the “Metformin” brand | MedDRA, WHODrug, Koda |
| Data Reconciliation | Make that all EDC, lab, PV, and device systems are consistent. | Reconciling QTc values in a cardiovascular study | SAE reconciliation tools |
| Data Cleaning and Review | Continuously clean data and get it ready for analysis. | Data lock time was shortened by 30% in an oncology study. | SAS, data listings |
| Compliance and Audit Readiness | Assure adherence to SOP, GCP, and Part 11. | Access to the audit trail is necessary for FDA inspections. | FDA 21 CFR Part 11, audit logs |
| Medical Writing and Collaboration with Stats | Encourage the growth of CSR, ADaM, and SDTM | CDISC-compliant files were provided by the Alzheimer’s study. | CDISC SDTM, AdaM |
| Regulatory Submission Report | Create datasets and guidelines that are ready for submission. | More than 300 datasets and reviewer documents in an NDA | Define.xml, eCTD Tools |
| Training and Site Enablement | Train sites on data quality and CRF completion. | Training with Veeva Vault EDC decreased entry mistakes. | SOPs, video modules |
| Risk-based Data Management | Prioritize high-risk websites and data using analytics. | Using the KRI dashboard, a vaccine experiment identified a dangerous spot. | Tableau, Spotfire, RBM systems |
Summary Table of Roles, Tools and Real-World Examples of Clinical Data Management
Conclusion
Every clinical trial’s effectiveness depends on the Clinical Data Management procedure. Every stage, from developing the protocol to locking the database, needs to be done precisely and legally.
As stewards of the data that powers medicine’s future, CDM experts are more important than ever in light of the growing complexity of trials and digital transformation.
Clinical Data Management is at the core of reliable, open, and timely clinical research, whether it is via data integrity, handling changing regulatory requirements, or incorporating next-generation technology.